VANDANA REDDY
BIMONTHLY INTERNAL ASSESSMENT FOR THE MONTH OF JANUARY 2021
More here: https://harikachindam7.
Case presentation links:
https://youtu.be/fz9Jssoc-mA
https://youtu.be/d4lLX04oL8s
https://youtu.be/CSCxw2zp7Oc
Pt has complaints since 1 month she has headache 1-2 times per week relieved on medication .but the headache worsened in the past 15 days .,
c/o Heaeache since 8 days- in bitemporal vertex region
has been aggrevated since 1 week .
After stopping using steroids she has
fever since 4 days- low grade not associated with chills and rigors.
vomitings since 1 week (multiple episodes).
She has generalised weakness,decreased apetite and unable to walk for
Neck pain since 4 days
At the time of presentation she has altered sensorium with irrelevant speech since 3 am in the morning
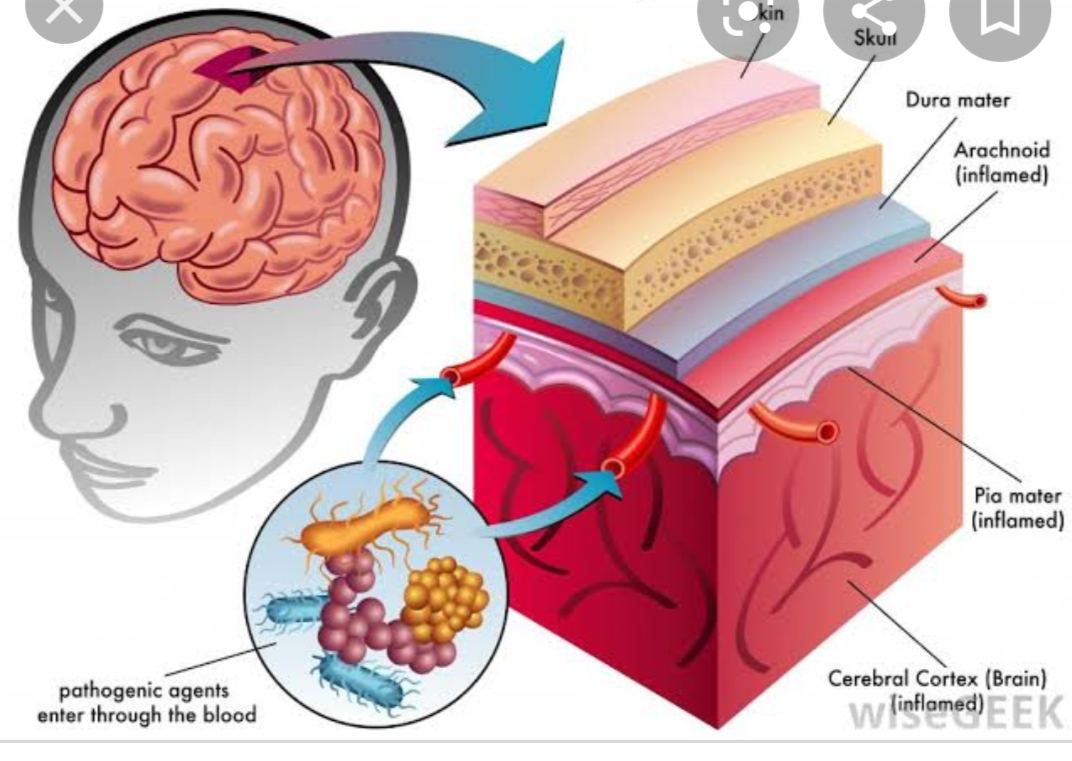
The anatomical location for her problems could be in meninges or brain parenchyma
c) What is the efficacy of each of the drugs listed in her prior treatment plan that she was following since last two years before she stopped it two weeks back?
Patient was on medication for SLE (Hydrochloroquine-200mg/OD,Sulfasalazine,Methylprednisolone,Alandronic acid and Cholecalciferol,Aceclofenac,Flupirtine,Gabapentine,Methylcobalamin tablets), which she stopped 10 days back.
https://pubmed.ncbi.nlm.nih.gov/8815753/d) Why was she given bisphosphonates?
What is the efficacy of using primary bisphosphonate prophylaxis for patients started on corticosteroids?
To assess the benefits and harms of bisphosphonates for the prevention and treatment of Glucocorticoid induced osteoporosis in adults.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6461188/?report=reader
It included
1. Prevention or treatment of Glucocorticoid induced osteoporosis
2. Adults taking a mean steroid dose of 5.0 mg/day or active treatment including bisphosphonates of any type alone or in combination with calcium or vitamin D
4) comparator treatment including a control of calcium or vitamin D, or both, alone or with placebo
Patients -
A total of 27 RCTs with 3075 participants in the review
- Pooled analysis for incident vertebral fractures included 12 trials (1343 participants)
Outcome - In this analysis 46/597 people experienced new vertebral fractures in the control group compared with 31/746 in the bisphosphonate group; relative improvement of 43% with bisphosphantes.
Basically BIPHOSPHONATES help in reducing osteoporosis
when used with steroids
Please share any reports around similar patients with SLE and TB meningitis?
Here's a case report of a 31 year old woman diagnosed with SLE and subsequently developed SLE myocarditis and Lupus Nephritis who also developed TB meningitis
https://pubmed.ncbi.nlm.nih.gov/28764615/
Another case report of a 51 year old woman with SLE who later developed TB meningitis
https://pubmed.ncbi.nlm.nih.gov/10067053/
e) What is the sensitivity and specificity of ANA in the diagnosis of SLE?
To determine the sensitivity and specificity of ANA and anti-dsDNA in SLE patients, using sera from Healthy controls and Multiple Medical problem patients.
The prevalence of ANA at a titer of ≥1:80 and ≥ 1:160 was 8% and 4%, respectively, in HC; and it was 12% and 6% respectively, in MMP patients. The prevalence of anti-dsDNA was 0% in HC and 3% in MMP patients. When using HC sera for the diagnosis of SLE, the sensitivity of ANA at a titer of ≥ 1:80 and ≥ 1:160 was 98% and 90%, respectively, with specificity of 92% and 96%, respectively. The specificity decreased to 88% and 94%, respectively, when using sera from MMP patients. The specificity of anti-dsDNA was 100% and 97%, when using sera from HC and MMP patients, respectively.
ANA and anti-dsDNA gave high sensitivity and high specificity in patients with SLE, even when using MMP patient's sera as controls.
https://pubmed.ncbi.nlm.nih.gov/24383972/
2.What was the research question in the above thesis presentation?
Could hypomagnesemia in type 2 DM lead to further more complications
b) What was the researcher's hypothesis?
According to the presenter, hypomagnesemia in type 2 diabetes mellitus could lead to further more complications and poor prognosis.
c)What is the current available evidence for magnesium deficiency leading to poorer outcomes in patients with diabetes?
Association of serum magnesium with Type 2 Diabetes Mellitus
https://youtu.be/jXVS5J1-RNE
3 .a)What was the research question in the above thesis presentation?
b)What was the researcher's hypothesis?
24 hours urinary sodium in newly diagnosed hypertensive patients
The hypothesis is that, the amount of salt consumed is almost equal to the sodium excreted in the urine, which could lead to increase in the blood pressure
c)What is the current available evidence for the utility of monitoring salt excretion in the hypertensive population?
Estimation of 24 hours urinary sodium excretion and relation to cardiovascular events
Salt restriction would certainly reduce the blood pressure and 24 hours urinary excretion of sodium does sound like a good way in measuring the salt intake but also it is important for blood pressure monitoring over 24 hours.
3.What is the efficacy of aspirin in stroke in your assessment of the evidence provided in the article. Please go through the RCT CASP checklist here https://casp-uk.net/casp-tools-checklists/ and answer the questions mentioned in the checklist in relation to your article.
Aspirin in the prevention of progressing stroke: a randomized controlled study
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2796.2003.01233.x
O - The main results of the trial showed that aspirin treatment did not significantly reduce the rate of stroke progression. The progression rate was 15.9% amongst patients treated with aspirin and 16.7% for those on placebo. In the aspirin group, the relative risk was 0.95 (95% CI 0.62–1.45).
1.i have seen a lady with frontal lobe mass with altered consciousness
5. i learned how to do plural tapping
.SLE with Tubercular meningitis
.Pancytopenia
.liver abscess with plural effusion
.peripheral vascular disease with supraventricular tachycardia
.pericardial effusion
5) a) What are the possible reasons for the 36 year old man's hypertension and CAD described in the link below since three years?
https://vamsikrishna1996.blogspot.com/2021/01/36-year-male-presented-to-casualty-at.html?m=1
The 36 year old man with CAD, the etiological reasons to his CAD could be due to the long standing hypertension since 3 years along with being an alcoholic and smoker since 15 years adds up to the risk factors.
b) Please describe the ECG changes and correlate them with the patient's current diagnosis.
The initial ecgs shows irregular rhythm along with VPS
There are progressive ST segment changes in the anteroseptal leads - ? STEMI involving LAD territory/ LAD aneurysm
c) Share an RCT that provides evidence for the efficacy of primary PTCA in acute myocardial infarction over medical management. Describe the efficacy in a PICO format.
jamanetwork.com/journals/jama/fullarticle/194837
Thrombolytic Therapy vs Primary Percutaneous Coronary Intervention for Myocardial Infarction in Patients Presenting to Hospitals Without On-site Cardiac SurgeryA Randomized Controlled TrialP - Four hundred fifty-one thrombolytic-eligible patients with acute MI of less than 12 hours' duration associated with ST-segment elevation on electrocardiogram.
225 received primary PTC
226 participants received accelerated tissue plasminogen activator (bolus dose of 15 mg and an infusion of 0.75 mg/kg for 30 minutes followed by 0.5 mg/kg for 60 minute
The incidence of the composite end point was reduced in the primary PCI group at 6 weeks (10.7% vs 17.7%) and 6 months (12.4% vs 19.9%) after index MI. Six-month rates for individual outcomes were 6.2% vs 7.1% for death, 5.3% vs 10.6% for recurrent MI, and 2.2% vs 4.0% for stroke for primary PCI vs thrombolytic therapy, respectively. Median length of stay was also reduced in the primary PCI group (4.5 vs 6.0 days)
Conclusions Compared with thrombolytic therapy, treatment of patients with primary PCI with better clinical outcomes for 6 months after index MI and a shorter hospital stay..sA


Comments
Post a Comment